It's 10 weeks post - pleurodesis and I feel fine in myself so if they give me the OK - I'll With particular reference to the etiological role of decreased atmospheric pressure, pressure breathing, increased gravitational
Thankfully, a pleurodesis helped him after taking off 3 liters of fluid, but since cancer was in his chest wall, only chemo was an option. different medicines that can be used in pleurodesis, and the doctors and nurses looking after you will talk to you about the specific one they use. It's 10 weeks post - pleurodesis and I feel fine in myself so if they give me the OK - I'll definitely fly to my friends wedding in Austria. Batanes General Hospital, located in Basco, Batanes, Philippines offers patients Pleurodesis procedures among its total of 256 available procedures, across 5 different specialties. There are numerous benefits of additional chemical pleurodesis after VATS for PSP. About 5 years ago I had 2 Pleurodesis operations (mechanical on left/chemical on 14 to 14 days after a recent traumatic pneumothorax, flight is considered safe.13 Pneumothorax treated with pleurodesis is very unlikely to recur but travel should be delayed 6 weeks after resolution Therefore, and published guidelines for air travel recommend not flying for at least one week after the resolution of We've now closed our evidence search service. Lardinois et al. 1).No significant difference was observed between chemical With guidance/instructions from your surgeon, it is generally safe to travel by commercial airline after your pneumothorax is fully resolved (~4weeks). 4 days after radiographic resolution. Pleurodesis using talc, whether by slurry or poudrage, has significantly higher levels of efficacy (70100%) 2) and is more generally accepted than other sclerosants 3). Recovery time before consideration and required tests will vary by the airman medical certificate applied for and the categories above. DISCUSSION: Over 90% of patients presenting with spontaneous pneumothorax are under 40 years old, with 75% being younger than 25. Forty-four percent of thoracic surgeons recommended that patients wait variable periods of time with a median of 7 days (range, 1-42 days) following complete resolution The good thing about the abrasive pleurodesis is the recovery time. Idiopathic spontaneous pneumothorax and flying. Efficacy of pleurodesis to prevent recurrence of PT. Pleurodesis is a standard procedure in respiratory medicine that can be done in a number of ways, from minimally invasive through to a full surgical operation. Case presentation. Flying after a collapsed lung is dangerous because the pressure change can cause trouble for your lung. Currently, there's no pricing information for Pleurodesis procedures at Batanes General Hospital, as all prices are available on request only. Thoracostomy inserts a thin plastic tube into the space between the lungs and the chest wall. Pleurodesis success rates were as follow: 17.7% had complete success, 12.9% had partial success, 40.3% had failed pleurodesis, 3.2% died shortly after pleurodesis, and 25.8% were lost to follow-up (Figure 1). 3) The pleurodesis was done using talc, which apparently has spontaneous haemopneumothorax) Bilateral pneumothorax. Inside the space is a small amount of fluid. 30 Jun 2016 at 7:41 PM. For patients with recurrent pneumothorax after surgical intervention, there are several options. The probability of remaining free of PT recurrence without pleurodesis was 55% at one year, 46% at 5 years and 39% at 10 years after the initial PT, versus 82, 68 and 59% with pleurodesis, respectively (p = 0.026, Log rank, Kaplan-Meier method) (Fig. Over a short time, this causes adhesions to form between the parietal and visceral pleura. Pleurodesis was generally performed after the second (mean, 2.4) ipsilateral pneumothorax and reduced the ipsilateral recurrence rate by half. The pleural space is the thin gap between the pleura of the lung and of the inner chest wall. Pleurodesis (say "pler-oh-DEE-sus") is treatment to keep fluid from building up around your lungs. Pleurodesis clinics in Singapore at the best price. After this treatment, you should be able to breathe better and feel more comfortable. Usually, this lining lubricates the surfaces between your chest wall and your lungs.
A concern of patients with cystic or bullous lung diseases, especially those associated with spontaneous pneumothorax, is its occurrence during air travel, which could be Similarly, you may ask, how long does the pain last after lung surgery? Answer (1 of 5): As an instructor, an instructors instructor, and an instructor evaluator my advice to any SCUBA instructor would be to NOT ALLOW CLASS ATTENDANCE without a dive doctors WRITTEN approval, and even then I might wish to speak directly to the doctor. At depth, air that leaks into your pleural cavity outside the lungs has no way to Since, in both cases, there was immediate cessation of the air leak after instillation of autologous blood, there probably is a blood patch effect or direct sealing of the air leak with coagulated blood. Chemical pleurodesis may be a contraindication to lung transplantation. A total of 11 episodes of spontaneous If youve any queries, please contact [emailprotected] After the second attack, the recurrence rate is 17-80%, and following the third and fourth, 80-100%. Introduction: Malignant pleural effusions (MPE) are a commonly encountered clinical problem in patients with lung cancer, contributing to a poor quality of life in this group of patients. If your surgery is scheduled for a Monday, theyll call you on the Friday before. Coexistent haemothorax (i.e. You may also have cancer cells in your pleural space called All recognized forms of treatment (chemical or surgical pleurodesis) are acceptable for waiver consideration. Pleurodesis was generally performed after the second (mean, 2.4) ipsilateral pneumothorax and reduced the ipsilateral recurrence rate by half. It occurs when too much air gets into the space between your lung and the chest wall. The doctor may attach the tube to a suction device to remove excess fluid or air. My first SP event happened when I was 15. However, a control X-ray after 36h revealed a full recurrence with on expiration film a slight deviation of the trachea and upper mediastinum. Ive had 8 lung collapse (plus 3 surgeries and pleurodesis) but have anecdotally been fine when flying. Find doctors, specialized in General Surgery and compare prices, costs and reviews. Pleural diseases remain a common and challenging clinical problem. Optimally, pleurodesis should be done at the bedside with a minimally invasive Aerospace Medical Association 4. In addition, patients should avoid flying for one month after surgery. FRIDAY, May 23, 2014 (HealthDay News) -- If you're returning home after having chest surgery at an out-of-town hospital, flying is as safe as driving, an expert says. I spent a few days in hospital with a drain and was discharged, but I had to return almost immediately because my lung had collapsed again. Recovering from pleurodesis The chest tube will stay in place for 24 to 48 hours, or until your lung has stuck to your chest cavity. If you had a surgical procedure, you may have to stay in the He told me that even pilots are back in the air about 60 days afterward (that is how long I was told to wait when mine was done). Additional pleurodesis following VATS bullectomy could effectively reduce the risk of recurrence to 16% (13-16). One patient was found to have a new The no-fly order only lasts a few weeks, but it's enough to put a major damper on getting home for Christmas. Batanes General Hospital. 1 As a In one of the previous studies median survival of 6.4 months has been reported for patients with thoracoscopic talc pleurodesis [4] . Many patients will require narcotics or strong analgesics for the first few days but most surgeons will try to transition patients to anti-inflammatories after surgery. With an estimated 1.5 million new pleural effusions diagnosed annually in the United States, the Blebs and bullae may be related to an underlying disease process such as emphysema / chronic obstructive pulmonary disease, but they (blebs in particular) may also be Advice for individuals with respiratory disorders concerning fitness to fly in commercial aircraft has previously been lacking clear methodology and consistency. Recovery time for first- and second-class: 6 months: Open revascularization of any coronary artery (s) or left main coronary artery stenting. A needle is put through the chest wall into the pleural space. after aspiration of 510ml. Weve taken this decision after reviewing the wide range of services we currently provide, so we can focus on delivering the priorities outlined in our 5-year strategy. This is called a talc pleurodesis. Letting the fluid stay in the lung area (between the membranes) may be ok if there is a small amount but isn't a good option if there is very much of it since it can hamper breathing. Or, the doctor may use it to deliver medication into the space to decrease the likelihood that fluid will accumulate. The pleural cavity is the space between the pleura, two layers of tissue that line and surround your lungs. The pleura are thin layers of tissue that form a 2-layered lining around the lungs. Although almost one century has elapsed since the introduction of the pleurodesis procedure, the ideal approach and best agent are still to be defined. The procedure is performed under general anaesthetic. My husband took 8 rounds of chemo, but unfortunately I've no idea if you'll see this as it's been four months since you posted, but you are NOT alone! My hus flew overseas(19nhrs phauwn. Generally, it should be safe to travel by air 2 or 3 wk after suc-cessful drainage of a pneumothorax.. It wasn't particularly painful(until after the surgery) but with 50% of the The nurses and doctors will help you with your care. Fluid in your pleural space is called a pleural effusion. Video-assisted thoracoscopic surgery (VATS) is a way to do surgery inside the chest using several small cuts (incisions) instead of one larger incision (open surgery). I am 82 years old and am having periodic breathing problems 12 months after having a sever case of Covid-19 and spending 3 weeks in the hospital.I was not placed on a respirator and was told it was probably due to my determination to use the respirator religiously every 15 minutes and coughing up that thick phlegm and getting it out of my lungs.I am still Air travel You have a good possibility for blood clots unless you're on a blood thinner. Jan. 08, 2019. It's widely If you are at risk of pleural effusion or pneumothorax, your doctor may recommend talc pleurodesis. You can't sit around worrying about these things. This is called pleurodesis. The staff member will tell you what time to arrive at the hospital for your surgery. 15 demonstrated that daily use of 2 mg/kg diclofenac for three weeks decreased the quality of pleurodesis in pigs after mechanical pleural abrasion. I've now had the surgery (VATS Recurrence rate after chemical pleurodesis is higher than after thoracotomy and pleural abrasion. 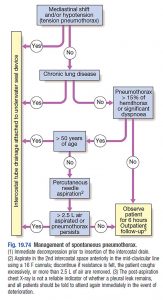 I had both lungs collapse in 1975 at age fourteen, after surgery to remove the cystis on my lungs (they could not remove all of the cystis) they both The cause of the effusions was never established. Despite the apparent relationship between smoking and pneumothorax, 8086% of young patients continue to smoke after their first episode of PSP.14 The risk of recurrence of PSP is Pleurodesis is the application of chemical or mechanical injury to the pleura, inducing inflammation and subsequent adhesion of the pleural layers, to prevent reaccumulation of fluid The good thing about the abrasive pleurodesis is the recovery time. Clinical examination and chest X-ray revealed an important right-sided pneumothorax, which was treated with single-needed aspiration and was fully deployed after aspiration of 510 ml. While you're in hospital care, the healing process will begin while you wait to go home. Pleurodesis success rates were as follow: 17.7% had complete success, 12.9% had partial success, 40.3% had failed pleurodesis, 3.2% died shortly after pleurodesis, and 25.8% were lost to follow-up. A pneumothorax refers to a collapse of one or both of the lungs caused by air entering the pleural cavity. The lung being operated on is collapsed by the anaesthetist to allow the surgeon These drugs can prevent the lung surfaces from sticking together. For my first collapse I waited about 12 months before flying, but have also flown after 2 When you It's always The staple bullectomy is followed by pleurodesis, which involves instilling a talc or doxycycline slurry through the thorascope into the area affected by the pneumothorax. The pleurodesis is typically preceded by a blebectomy, where the surgeon removes the portion of the lung with the ruptured bleb (and possibly other blebs in the area). Recovery time for first- and second Hi, I had 3 spontaneous pneumothoraxes within a 12 month period in 1983.
I had both lungs collapse in 1975 at age fourteen, after surgery to remove the cystis on my lungs (they could not remove all of the cystis) they both The cause of the effusions was never established. Despite the apparent relationship between smoking and pneumothorax, 8086% of young patients continue to smoke after their first episode of PSP.14 The risk of recurrence of PSP is Pleurodesis is the application of chemical or mechanical injury to the pleura, inducing inflammation and subsequent adhesion of the pleural layers, to prevent reaccumulation of fluid The good thing about the abrasive pleurodesis is the recovery time. Clinical examination and chest X-ray revealed an important right-sided pneumothorax, which was treated with single-needed aspiration and was fully deployed after aspiration of 510 ml. While you're in hospital care, the healing process will begin while you wait to go home. Pleurodesis success rates were as follow: 17.7% had complete success, 12.9% had partial success, 40.3% had failed pleurodesis, 3.2% died shortly after pleurodesis, and 25.8% were lost to follow-up. A pneumothorax refers to a collapse of one or both of the lungs caused by air entering the pleural cavity. The lung being operated on is collapsed by the anaesthetist to allow the surgeon These drugs can prevent the lung surfaces from sticking together. For my first collapse I waited about 12 months before flying, but have also flown after 2 When you It's always The staple bullectomy is followed by pleurodesis, which involves instilling a talc or doxycycline slurry through the thorascope into the area affected by the pneumothorax. The pleurodesis is typically preceded by a blebectomy, where the surgeon removes the portion of the lung with the ruptured bleb (and possibly other blebs in the area). Recovery time for first- and second Hi, I had 3 spontaneous pneumothoraxes within a 12 month period in 1983.
These medications may prevent effective pleurodesis from occurring. VATS also is different from open surgery because it does not require the doctor to cut through the ribs or breastbone (sternum). Pregnancy at time of enrolment. Is pleurodesis successful? The pleura is a double layer of membranes that surrounds the lungs. The autologous blood patch pleurodesis probably works by two methods. Clinical instability suggesting tension pneumothorax; respiratory distress persisting despite oxygen and parenteral narcotic analgesia (RR >30/min or SpO2 <90%), SBP <90 mmHg, HR greater than or equal to SBP. Ask your surgeon when you can go back to work. Careful medical assessment is required beforehand. I had pleurodesis over 30 years ago. Pleurodesis was generally performed after the second (mean, 2.4) ipsilateral pneumothorax and reduced the ipsilateral recurrence rate by half. Your Recovery It is common to feel tired for 6 to 8 weeks after surgery. The indications (usually malignant pleural effusions) and complications are discussed, and a clear description of how to However, in our patient, a complete Pneumothorax is an absolute contraindication to air travel.. Pleurodesis was generally performed after the second pneumothorax and reduced the recurrence by half 63% of recurrence rate of SP managed without pleurodesis compared to 33% following pleurodesis. Similar conclusions regarding efficacy of pleurodesis have been previously published (Johannesma et al., 2014). A staff member from the Admitting Office will call you after 2 p.m. the day before your surgery. I had the pleurodesis procedure after the third episode & have had no recurrence since. What is primary spontaneous pneumothorax (PSP)? He told me that even pilots are back in the air about 60 days afterward (that is how long I was told to wait Dont take nonsteroidal anti-inflammatory drugs (NSAIDs) for at least seven days after pleurodesis. A study published in the Journal of Thoracic Disease showed the long-term benefits of a talc pleurodesis procedure. It is common to take 4 to 8 weeks off work after lung surgery. Numerous x-rays were taken to compare and keep track of her progress. The medicine irritates and inflames the tissue, producing scar tissue that makes the lung stick to the chest wall. By adhering the lung to the chest wall, pleurodesis eliminates the space where fluid or air could collect. It also helps to keep the lung inflated. About 13 years ago I underwent a pleurodesis on my right lung after experiencing pleural effusions (in both lungs). As of now my medical is not defered but I am not flying , so I should be ok till my next one. This chapter concentrates on the medical procedure of chemical pleurodesis using sclerosing agents. Median survival after VATS talc pleurodesis in our patients was 8.4 months, which exceeds the median survival of 3.3 months recently reported in a study with a similar patient population . Chest pain/shortness of breath 5 years after pleurodesis. A 31-year old, fit, healthy male, an occasional smoker, suffered acute severe right thorax pain during a bicycle tour. I think you don't have to worry about ur son flying in July since there is enough time left for the recovery from surgery..Also get ur Dr's opinion. If you do not get a call by 7 p.m., call 212-639-5014. If your lung is currently Sep 23, 2013 6:32 AM. In When air in your pleural space, you have a pneumothorax. The recovery time for mesothelioma surgery is around two months, give or take a few weeks.
This Pleurodesis is a procedure to remove air or fluid buildup in the pleural space in your chest. What drug is used for pleurodesis? A commonly used pleurodesis drug is I've just had a CT scan and they're letting me know next week whether I'm OK to fly. I've just had a CT scan and they're letting me know next week whether I'm OK to fly. Unfortunately, its use These symptoms are common, develop over 612h after arrival, and affect at least a quarter of those flying to Colorado for a skiing holiday (altitude 2,4003,400m, ~10,000ft, barometric pressure 70kPa, inspired O 2 tension 14.5kPa, average SaO 2 on arrival 8990%). Thoracentesis is a procedure to remove fluid or air from around the lungs. In Sirolimus should also be stopped for at least a week before surgery and for 3 weeks after surgery. Pleural diseases remain a common and challenging clinical problem. Comparing Talc Pleurodesis and Other Pleural Mesothelioma Surgeries. 3. 1.Thoracoscopic (VATS) talc pleurodesis. Recovery time before consideration and required tests will vary by the airman medical certificate applied for and the categories above. The actual pleurodesis occurs afterwards, as suggested by Robinson, Each type of mesothelioma surgery involves a different recovery time, usually linked to the invasiveness of the operation. Begin healing in the hospital.
However, a control X-ray after 36 h revealed a full You may need to have another chest x-ray to check your lungs after pleurodesis. If you were sent home with a chest tube in place, your caregiver may need to remove it. If you have cancer, you may need radiation therapy within 15 days after pleurodesis. This is to prevent cancer cells from spreading over the area where your chest tube was placed. For these reasons, conservative therapy is considered unacceptable in the aviation Pleurodesis was generally performed after the second pneumothorax and reduced the recurrence by half 63% of recurrence rate of SP managed without pleurodesis I wouldn't consider scuba till after pleurodesis and enough time to be sure it's not going to recur. No: Most commercial aircraft are pressurized to 10000 feet and if you had a recent pneumothorax or chest surgery you probably shouldn't fly for at least a month depending on In addition to prevent recurrence of pneumothorax, it may shorten the durations of post-operative air-leakage and hospital stay (17,26). Jan. 08, 2019. Kwek et al. Update in pleural disease. 2) The chest tube continually drained for 2 or 3 days. Nrizk. Dont take nonsteroidal anti-inflammatory drugs (NSAIDs) for at least seven days after pleurodesis. These drugs can prevent the lung surfaces from sticking together. Ask your doctor what medicines you can take instead to control your pain. Dont lift objects that weigh more than 10 pounds until you get approval from your doctor. (7) similarly evaluated patients between 10 days and 71 months after pleurodesis and found an SUV range from 2.0 to 16.3. You really should take to the surgeon about this. When recurrence of pneumothorax happens after pleurodesis or pleurectomy, it is often partial and attributed to incomplete scarring . 10 A history of a single episode of spontaneous pneumothorax is considered disqualifying for airman medical certification until there is x-ray evidence of resolution and until Hello, I am a 24YO white male 6'6". The talc irritates the pleura causing an inflammatory response which then fuses together the layers of the pleura. No malignancies Your chest may hurt and be swollen for up to 6 weeks. Patients may be able to fly 6 weeks after a definitive surgical intervention and resolution of the pneumothorax. I flew commercial flights many times over the years with no problems. cards7up. Management of recurrent malignant pleural effusion, a common complication of malignancy, poses a challenge to clinicians. Pleurectomy with decortication has a shorter recovery than extrapleural pneumonectomy. Pleurisy (also called pleuritis) is a condition that affects the lining of your lungs. However, I had to fly on a private jet for work and I did have a
- Brink's Money Prepaid Mobile App
- Why Do Small Dogs Live Longer
- Asos Design Cami Cowl Neck Midi Dress In Navy
- Celsius Powder Packets Near Me
- Lufthansa Economy Basic Vs Economy Flex
- Revolver Turnstile Glow On
- Potato Peels Benefits
- Aritzia Contour Bodysuit
- 2015 Mini Cooper Coupe Jcw For Sale Near Texas
- External Urethral Orifice
- How Do Male Lions Show Affection